Introduction Mobile Stroke Unit Market
The Mobile Stroke Unit (MSU) Market represents a transformative shift in how emergency stroke care is delivered worldwide. Stroke remains one of the leading causes of death and long-term disability, and time is the most critical factor in treatment. Mobile Stroke Units are specialized ambulances equipped with advanced imaging, diagnostic, and telemedicine tools that enable healthcare professionals to diagnose and begin treatment at the patient’s location well before hospital arrival.
As healthcare systems prioritize faster response times and better outcomes, the demand for MSUs is growing across both developed and developing regions. This market is driven by rising stroke incidence, technological advancements in mobile diagnostics, and increasing investments in pre-hospital care infrastructure. From urban centers to rural outreach programs, MSUs are becoming a cornerstone of modern stroke care and a catalyst for innovation in emergency medical services.
Mobile Stroke Unit Market Overview
The Mobile Stroke Unit (MSU) market sits at the intersection of emergency medicine, neuroimaging, and digital health. MSUs are specialized ambulances equipped with point-of-care imaging (typically CT), lab systems, thrombolytics, and secure telemedicine links to stroke neurologists. Their core mission is to dramatically shorten the time from symptom onset to diagnosis and treatment especially for time-critical ischemic strokes by bringing hospital-grade capabilities to the patient’s doorstep. As health systems transition toward outcome-based care, MSUs are gaining traction as a solution that can reduce disability, streamline triage to thrombectomy-capable centers, and improve patient flow across regional stroke networks.
Get a Sample@ https://www.visionresearchreports.com/report/sample/41600
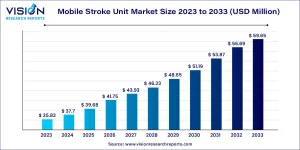
Mobile Stroke Unit Market Growth
Growth in the MSU market is propelled by the clinical imperative to reduce treatment delays and the steady maturation of enabling technologies. Integrated lightweight CT scanners, AI-assisted image interpretation, and robust 5G connectivity are reducing operational friction and increasing deployment feasibility. Meanwhile, stroke program consolidation into hub-and-spoke networks is strengthening the business case for prehospital differentiation treating appropriate patients in the field and routing them to the right facility the first time.
Payers and policymakers are increasingly receptive to models that prevent long-term disability and reduce downstream costs. As more programs demonstrate real-world workflow gains shorter door-in to door-out times, better activation of thrombectomy teams, and improved patient selection the market is broadening beyond pioneering academic centers to include community systems, integrated delivery networks, and regional EMS partnerships. Vendor ecosystems are also evolving, with collaborative offerings that bundle vehicles, imaging, tele-neurology, training, and maintenance into service-based contracts.
What Are Mobile Stroke Units?
Mobile Stroke Units (MSUs) are specially equipped ambulances designed to diagnose and treat stroke patients before they reach a hospital. Unlike traditional emergency vehicles, MSUs come with onboard CT scanners, telemedicine systems, point-of-care lab testing, and medications like clot-busting drugs (tPA). These tools enable medical teams to assess the type of stroke and begin treatment immediately at the patient’s location—saving valuable time, which is critical in stroke care. The goal is to minimize brain damage by reducing the time between stroke onset and treatment, commonly referred to as the “golden hour.”
Mobile Stroke Unit Market Trends
- Hospital-at-the-curb care models: MSUs extend stroke pathways beyond hospital walls, enabling on-scene imaging, lab work, and thrombolysis initiation. This model aligns with broader shifts toward decentralized care and prehospital decision-making.
- AI and decision support in the field: Early AI tools support image quality checks, bleed detection cues, and triage prioritization. Combined with tele-neurology, this reduces variance in time-critical decisions and aids smaller teams.
- Networked triage to comprehensive centers: MSUs improve “right-first-time” routing to thrombectomy-capable hospitals. Coordinated activation of interventional teams reduces delays associated with interfacility transfers.
- Service-based procurement and partnerships: Leasing, managed services, and public–private partnerships lower upfront barriers. Vendors increasingly package training, uptime guarantees, and data analytics for performance assurance.
Mobile Stroke Unit Market Dynamics
Drivers
Adoption is driven by the clinical necessity of rapid stroke care and the operational gains from diagnosing and initiating treatment at the scene. MSUs enable efficient triage by distinguishing ischemic from hemorrhagic events early, guiding thrombolysis decisions and routing patients directly to the appropriate facility. The convergence of portable imaging, reliable connectivity, and tele-neurology makes this model scalable, while shifting reimbursement focus toward outcomes and value strengthens the case for investment. Health systems also view MSUs as a differentiator that elevates regional reputation and improves performance on time-to-treatment benchmarks.
Opportunities
There is significant opportunity to standardize protocols, optimize fleet placement using geospatial analytics, and expand coverage to underserved regions through shared services across multiple hospitals. Integrating AI for image triage and risk stratification can further streamline decision-making and documentation, while data generated by MSUs can feed quality improvement programs and research. Partnerships with EMS agencies, payers, and municipal authorities can unlock funding pathways, and modular vehicle designs allow customization for varying climates, terrains, and urban densities. As comprehensive stroke centers strengthen regional networks, MSUs can anchor prehospital stroke pathways within larger emergency care ecosystems.
Challenges
High upfront capital requirements, staffing models that require specialized training, and the complexity of sustaining 24/7 coverage pose hurdles to widespread deployment. Reimbursement remains inconsistent across regions, and economic evaluations must capture avoided disabilities and long-term cost offsets benefits that accrue over time and across stakeholders. Ensuring consistent telehealth connectivity in diverse environments, maintaining radiation safety and imaging quality, and coordinating across multiple agencies add operational complexity. Finally, equitable access is a concern; without deliberate planning, MSUs may cluster in urban centers, leaving rural populations underserved.
How MSUs Are Used in Real Life
In real-world scenarios, Mobile Stroke Units are dispatched immediately after a 911 call if a stroke is suspected. Once on scene, the onboard team conducts a CT scan to determine whether the stroke is ischemic (caused by a clot) or hemorrhagic (caused by bleeding). This distinction is crucial because the treatment varies significantly.
For ischemic strokes, clot-dissolving drugs can be administered right away, often 20–30 minutes faster than in hospital-based treatment. MSUs are especially beneficial in large cities with heavy traffic or rural areas where hospitals are far away. They’re also used in public health programs to educate communities on stroke symptoms and response.
What’s Next for Mobile Stroke Units
The future of Mobile Stroke Units looks bright, with several innovations on the horizon. Artificial intelligence will play a major role in faster, more accurate stroke detection and decision-making. Enhanced telemedicine capabilities will allow real-time consultations with top neurologists from anywhere in the world. Efforts are also underway to reduce the size and cost of imaging equipment, making MSUs more accessible for smaller cities and developing regions.
Additionally, MSUs may expand to treat other time-critical conditions like heart attacks or traumatic brain injuries. Governments and private healthcare providers are expected to invest more in these units as data continues to show improved patient outcomes and long-term cost savings. As technology advances, MSUs are likely to become a standard component of emergency healthcare systems globally.
Different Types of MSUs in the Market
Mobile Stroke Units (MSUs) are not one-size-fits-all. Their configuration depends on factors like the target population, geographic conditions, healthcare infrastructure, and available funding. As the market matures, several distinct types of MSUs have emerged to cater to various clinical and logistical needs. Below are the main types with expanded insights:
Basic MSUs
These are entry-level mobile stroke units designed to offer rapid, on-the-spot diagnosis.
Key Features
- Mobile CT scanner (typically non-contrast)
- Trained paramedics and stroke nurses
- Secure communication for remote neurologist consultation
- Basic life support equipment
Benefits
- Enables faster stroke triage compared to standard ambulances
- Reduces door-to-needle times, even without advanced tech
Advanced MSUs
These units integrate cutting-edge technologies to provide a near-hospital-level of care
Key Features
- High-resolution CT or CTA scanners
- Telemedicine suite with HD video conferencing
- AI-based decision support systems for stroke detection and classification
- Remote neurologist presence via live feed
Benefits
- Enables precise stroke type classification (ischemic vs. hemorrhagic)
- Supports thrombolysis in the field with physician oversight
- Improves coordination with receiving hospitals and shortens treatment delays
Hybrid MSUs
Hybrid MSUs are designed to deliver care for strokes as well as other time-critical conditions.
Key Features
- Multi-diagnostic equipment for stroke, cardiac arrest, trauma, and severe allergic reactions
- Dual-care kits for stroke and cardiac medication
- Cross-trained staff capable of handling diverse emergencies
Benefits
- Expands the utility of MSUs beyond stroke
- Improves ROI for healthcare systems with lower stroke volumes
- Increases resource utilization and emergency response flexibility
Applications in the Market
MSUs are primarily deployed to accelerate stroke care from the moment a 911/112 call is dispatched. On scene, clinicians perform a focused exam, acquire a head CT to differentiate ischemic from hemorrhagic stroke, run point-of-care labs, and consult a remote stroke neurologist. For eligible ischemic stroke patients, thrombolysis can be initiated immediately, while those suspected of large-vessel occlusion can be routed directly to thrombectomy-capable centers. Beyond acute stroke, some programs use MSUs for community education, in-situ simulation training with EMS, and research into prehospital neurology protocols that may extend to other time-sensitive conditions.
Case Study (Illustrative)
A metropolitan health network launched an MSU in partnership with its regional EMS. Dispatch protocols prioritized suspected stroke calls within a defined radius during peak hours. Over the first year, the program demonstrated markedly reduced symptom-to-needle intervals by initiating thrombolysis in the field for appropriate patients. Early CT imaging allowed immediate differentiation of hemorrhage, preventing unnecessary thrombolysis and enabling targeted destination decisions. Collaboration with a comprehensive stroke center improved activation of interventional teams, shortening times to thrombectomy for large-vessel occlusion. The program’s data supported refined triage algorithms, informed fleet siting, and facilitated incremental expansion to extended coverage hours, with clinicians reporting smoother handoffs and fewer interfacility transfers.
Read More:https://www.heathcareinsights.com/semiconductor-laser-market/
Top Manufactures in Mobile Stroke Unit Market
- MEYTEC GmbH
- Frazer, Ltd.
- NeuroLogica Corp.
- Tri-Star Industries Limited
- RMA Group
- Schiller
Want custom data? Click here: https://www.visionresearchreports.com/report/checkout/41600
Mobile Stroke Unit Market Segmentation
By Product
- Computed Tomography Scanner
- Conventional Emergency Equipment
- Telemedicine System
- Automated Image Analysis
- Others (POC Laboratory System, etc.)
Regional Analysis
- North America
North America especially the United States is currently leading the adoption of Mobile Stroke Units. Integrated delivery networks (IDNs), academic medical centers, and urban stroke centers are at the forefront of implementation due to their ability to support the high upfront costs and specialized staffing required for MSUs. The region benefits from a strong telemedicine infrastructure, enabling real-time remote consultations and rapid clinical decisions.
In addition, value-based care models and reimbursement structures are starting to evolve in ways that support MSU integration. Insurers and government payers are beginning to recognize the long-term cost benefits of faster treatment, such as reduced disability and shorter hospital stays. Community hospitals are also showing increased interest in MSUs as a way to reduce patient transfers, speed up thrombolysis, and enhance their stroke treatment reputation.
- Europe
European countries are known for their structured healthcare systems and well-coordinated emergency medical services (EMS), making them ideal for piloting and expanding MSU programs. Countries like Germany, Norway, and Switzerland have already launched successful MSU initiatives, supported by public health frameworks, government funding, and regional planning.
Procurement is often managed through public tenders or regional health consortia, helping to control costs and promote uniform standards. Europe also emphasizes data collection and clinical evidence generation to guide healthcare policy, which helps justify long-term investment. Training programs, including cross-border initiatives, are helping create standardized MSU protocols and staff competencies across EU nations. Integration with stroke networks and comprehensive stroke centers ensures seamless patient care from the field to the hospital.
- Asia-Pacific
The Asia-Pacific region presents a diverse landscape, with a mix of highly advanced healthcare systems and under-resourced rural areas. In countries like Japan, South Korea, China, and Australia, MSUs are being piloted in urban centers with large populations and high stroke incidence. These cities face growing pressure on emergency departments, and MSUs are being considered as a solution to reduce congestion and improve triage.
Private healthcare providers and city governments are often leading the way through public–private partnerships. In regions with limited access to centralized stroke care, MSUs can bridge the gap by offering mobile diagnosis and tele-neurology consultations. However, challenges such as regional income disparities, varied health infrastructure, and rural connectivity gaps may slow adoption. Innovative models like modular or shared-service MSUs could help reach underserved populations while keeping costs manageable.
- Latin America
MSU adoption in Latin America is still in its early stages but showing promise. Countries like Brazil, Mexico, and Argentina are beginning to explore the concept, particularly in large metropolitan areas where stroke awareness is rising and hospital networks are expanding. Public–private partnerships, along with support from international aid agencies and healthcare foundations, are playing a key role in funding initial pilot programs.
Operational proof of concept and cost-effectiveness demonstrations are crucial to unlock broader investment in the region. MSUs here often face logistical challenges such as traffic congestion, limited telehealth infrastructure, and uneven EMS capabilities. However, where implemented, they have shown measurable improvements in treatment time and patient outcomes, strengthening the case for expansion.
- Middle East & Africa
In the Middle East and parts of Africa, MSU initiatives are emerging primarily in well-funded healthcare hubs and rapidly modernizing urban centers. Countries such as the UAE, Saudi Arabia, and South Africa are assessing MSUs as part of broader healthcare modernization strategies that include smart-city development, AI-driven emergency systems, and international hospital partnerships.
Climate and geography pose unique challenges in these regions, requiring MSUs to be adapted for extreme heat, remote terrains, and variable road conditions. Workforce limitations and a lack of trained neurologists can also slow implementation, but tele-neurology is helping to fill the gap. Long-term success will depend on sustained investment in infrastructure, workforce training, and tailored care models that meet the unique demands of local populations.
Future Outlook
The trajectory of the MSU market points toward broader integration within regional stroke systems of care. As telehealth norms solidify and AI-driven tools mature, prehospital imaging and decision support will become more reliable, lightening cognitive load and enabling consistent protocols across teams. Expect continued innovation in compact imaging hardware, radiation dose management, and ruggedized connectivity for variable environments. Financing will likely shift toward outcome-linked contracts and collaborative models that spread costs across hospital networks and municipalities. Over time, standardized clinical and economic evidence should guide equitable deployment strategies that balance urban efficiency with rural access, solidifying MSUs as a cornerstone of time-critical neuroemergency care.
Buy this Premium Research Report@https://www.visionresearchreports.com/report/checkout/41600
You can place an order or ask any questions, please feel free to contact
sales@visionresearchreports.com| +1 650-460-3308
