The global AI in revenue cycle management market size was estimated at around USD 20.67 billion in 2024 and it is projected to hit around USD 180.53 billion by 2034, growing at a CAGR of 24.20% from 2025 to 2034.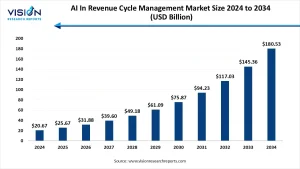
Get a Sample@https://www.visionresearchreports.com/report/sample/41664
AI in Revenue Cycle Management Market Overview
Artificial Intelligence (AI) is reshaping the healthcare industry, and one of its most transformative applications lies in Revenue Cycle Management (RCM). RCM encompasses the financial processes that healthcare facilities use to track patient care episodes from registration and appointment scheduling to the final payment of a balance. AI, with its capabilities in automation, data analysis, and predictive modeling, is streamlining these processes to enhance efficiency, reduce human error, and increase revenue recovery.
AI In Revenue Cycle Management Market Growth
The rising adoption of electronic health records (EHR), increased complexity in medical billing, and a growing emphasis on minimizing claim denials are accelerating the implementation of AI in RCM. Healthcare providers are under pressure to maintain financial viability amid tightening regulations and reimbursement challenges. AI offers predictive analytics, automated coding, and smart billing tools that significantly cut down administrative overhead and enhance financial accuracy.
Labor shortages and increasing operational costs are prompting healthcare systems to turn to AI as a strategic lever for cost containment and process improvement. As AI algorithms become more advanced, they are being used not only for automating mundane tasks but also for strategic forecasting and risk scoring, further embedding AI within the financial fabric of healthcare institutions.
AI In Revenue Cycle Management Market Dynamics
Drivers
- Increasing healthcare data volume and complexity.
- Need for cost containment and operational efficiency.
- Rising prevalence of chronic diseases leading to increased patient visits and billing volume.
Restraints
- High initial cost of AI implementation.
- Concerns over data privacy and cybersecurity in healthcare settings.
Opportunities
- Integration of AI with blockchain for secure and transparent transactions.
- Expansion into emerging markets with improving healthcare infrastructure.
AI In Revenue Cycle Management Market Size Market Trends
- Automation of repetitive tasks such as claims processing and billing reduces the burden on administrative staff and accelerates revenue flow.
- Predictive analytics and machine learning are being used to forecast patient payment behavior and optimize collection strategies.
- Natural language processing (NLP) helps in extracting billing information from clinical notes, improving coding accuracy.
- Integration with telehealth and remote care platforms ensures real-time billing and reduces errors in documentation.
Case Study: Northwell Health
Northwell Health, one of New York’s largest healthcare providers, implemented an AI-driven RCM platform to address inefficiencies in claims management and reduce denial rates. The system leveraged predictive analytics to flag claims likely to be denied and provided real-time alerts for missing or incorrect documentation. As a result, the organization reported a 30% reduction in claim denials and a 15% increase in overall revenue within the first year of deployment, demonstrating the tangible ROI of AI in RCM.
Read More:https://www.heathcareinsights.com/bioconjugation-market/#Future_Outlook
Top Companies in AI In Revenue Cycle Management Market
- Optum (UnitedHealth Group)
- Cerner Corporation (now part of Oracle)
- Epic Systems Corporation
- McKesson Corporation
- Change Healthcare
- Athenahealth (a Veritas Capital portfolio company)
- Waystar
- R1 RCM Inc.
- IBM Watson Health
- Cognizant Technology Solutions
AI In Revenue Cycle Management Market Segments
By Component
- Software
- Services
By Deployment Mode
- On-premise
- Cloud-based
By End-user
- Hospitals
- Physician Clinics
- Diagnostic Laboratories
- Ambulatory Surgical Centers
By Application
- Claims Management
- Medical Coding & Billing
- Payment Processing
- Patient Eligibility Verification
- Revenue Integrity
Future Outlook
As healthcare continues to digitalize, AI’s role in RCM is poised to become more central and strategic. Future advancements may include hyper-personalized billing systems, AI-powered virtual assistants for financial counseling, and real-time fraud detection tools. With regulatory bodies also warming to AI-backed processes, especially those that improve patient satisfaction and financial transparency, the coming decade will likely see a surge in innovation and adoption across healthcare ecosystems
Buy this Premium Research Report@https://www.visionresearchreports.com/report/checkout/41664
You can place an order or ask any questions, please feel free to contact
sales@visionresearchreports.com| +1 650-460-3308
